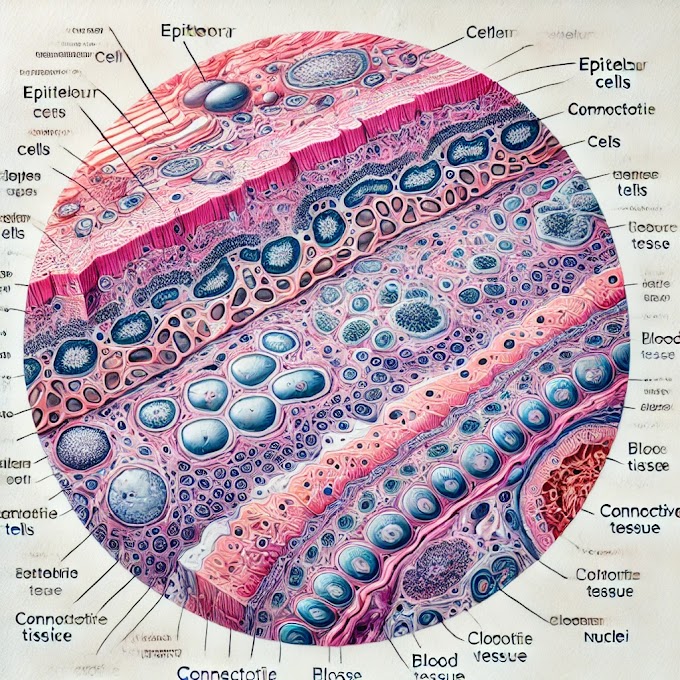
Histology slide of the parathyroid gland, here are the key identification points to focus on:
1. Chief Cells (Principal Cells)
- Appearance: Chief cells are the most abundant cells in the parathyroid gland. They are small, polygonal cells with centrally located, round nuclei.
- Cytoplasm: The cytoplasm is relatively dark and stains basophilic (blue or purple) with hematoxylin and eosin (H&E) staining.
- Function: These cells produce parathyroid hormone (PTH), which regulates calcium and phosphate balance in the blood.
2. Oxyphil Cells
- Appearance: Oxyphil cells are larger and less numerous than chief cells. They usually appear in small clusters, particularly in older individuals.
- Cytoplasm: The cytoplasm stains eosinophilic (pink or red) and appears lighter than that of chief cells, due to an abundance of mitochondria.
- Function: The exact function of oxyphil cells is not fully understood, though they are thought to support chief cells or may serve a reserve function.
3. Adipose Tissue (Fat Cells)
- Appearance: In adults, fat cells are often present within the parathyroid gland and increase with age.
- Location: Scattered throughout the gland, they appear as large, empty-looking cells due to the lipid content being removed during slide preparation.
4. Blood Vessels
- Appearance: The parathyroid gland is highly vascularized, with small blood vessels seen between clusters of chief cells and oxyphil cells.
- Function: Blood vessels supply the gland with nutrients and facilitate the release of PTH into the bloodstream.
5. Fibrous Septa
- Appearance: Thin connective tissue partitions, or septa, may divide the parathyroid tissue into small lobules.
- Function: These septa provide structural support and contain blood vessels and nerves.
Overall Slide Identification Points
When identifying the parathyroid gland on a histology slide, look for:
- Dense clusters of small, basophilic-staining chief cells.
- Scattered clusters of larger, lighter-staining oxyphil cells.
- Some adipose tissue, especially in slides of adult parathyroid.
- Numerous small blood vessels among cell clusters.
These features differentiate the parathyroid gland from the adjacent thyroid tissue, which typically shows large colloid-filled follicles.
Anatomy of the Parathyroid Glands
- Location: The parathyroid glands are typically four small, oval-shaped glands located on the posterior surface of the thyroid gland. They are usually about the size of a grain of rice and are found in pairs (two on each side).
- Structure: Each gland has a thin connective tissue capsule surrounding it, and within the gland, cells are organized into clusters or cords. The main cell types are chief cells and oxyphil cells.
Physiology of the Parathyroid Glands
The primary function of the parathyroid glands is to regulate calcium and phosphate homeostasis through the secretion of parathyroid hormone (PTH).
Parathyroid Hormone (PTH):
- Calcium Regulation: PTH increases blood calcium levels by acting on bones, kidneys, and the intestines.
- In Bones: PTH stimulates osteoclasts to break down bone tissue, releasing calcium into the blood.
- In Kidneys: PTH enhances calcium reabsorption and stimulates the kidneys to produce active vitamin D (calcitriol), which increases calcium absorption in the intestines.
- In Intestines: PTH indirectly increases calcium absorption by promoting the activation of vitamin D.
- Phosphate Regulation: PTH decreases blood phosphate levels by reducing phosphate reabsorption in the kidneys, causing more phosphate to be excreted in urine.
- Calcium Regulation: PTH increases blood calcium levels by acting on bones, kidneys, and the intestines.
Calcitonin Interaction: While PTH raises blood calcium levels, calcitonin (from the thyroid gland) lowers blood calcium, creating a balance.
Histology of the Parathyroid Glands
Chief Cells:
- Small, basophilic cells responsible for synthesizing and secreting PTH.
- Organized in cords or clusters, with a dark-staining appearance due to their dense nuclei and cytoplasmic basophilia.
Oxyphil Cells:
- Larger than chief cells, with eosinophilic cytoplasm and fewer in number.
- Their exact function remains uncertain, but they may serve a supportive or backup role in hormone production.
Adipose Tissue:
- Fat cells are commonly interspersed among the cells of the parathyroid, especially in adults.
Vascularization:
- The glands are highly vascular to facilitate quick release of PTH into the bloodstream when calcium levels fall.
Histopathology of the Parathyroid Glands
Histopathological examination of the parathyroid glands helps identify several diseases:
Hyperparathyroidism:
- Primary Hyperparathyroidism: Caused by an adenoma, hyperplasia, or, less commonly, carcinoma in the parathyroid glands, leading to excessive PTH production and hypercalcemia. Histology may show an enlarged gland with proliferated chief cells.
- Secondary Hyperparathyroidism: Often a result of chronic kidney disease, where the glands are overactive in response to low calcium levels. Histology shows hyperplasia of the parathyroid cells.
- Tertiary Hyperparathyroidism: Seen in long-standing secondary hyperparathyroidism where the parathyroid becomes autonomously overactive, even when calcium levels are normalized.
Hypoparathyroidism:
- Often due to surgical removal of the parathyroid glands or autoimmune destruction, leading to insufficient PTH production and hypocalcemia. Histology may show reduced or absent parathyroid tissue.
Parathyroid Carcinoma:
- Rare cancer of the parathyroid glands. Histology can show invasive growth patterns, mitotic figures, and atypical cells.
Clinical Significance of the Parathyroid Glands
Calcium Imbalance:
- Hypercalcemia: High blood calcium levels due to excessive PTH can lead to kidney stones, osteoporosis, abdominal pain, and neuromuscular symptoms. It is often caused by primary hyperparathyroidism or tertiary hyperparathyroidism.
- Hypocalcemia: Low blood calcium due to inadequate PTH (e.g., from hypoparathyroidism) leads to symptoms like muscle cramps, tetany, numbness, and potentially life-threatening cardiac issues.
Bone Health:
- Chronic overproduction of PTH can cause weakened bones (osteopenia or osteoporosis), increasing fracture risk due to increased bone resorption.
Renal Health:
- Secondary hyperparathyroidism, common in chronic kidney disease, can exacerbate kidney function issues and mineral imbalances, contributing to a condition called renal osteodystrophy.
Endocrine and Autoimmune Disorders:
- Parathyroid disorders may coexist with other endocrine or autoimmune diseases, particularly in genetic syndromes like multiple endocrine neoplasia (MEN) syndromes, where parathyroid adenomas are common.
Summary
The parathyroid glands are vital for maintaining calcium balance, with PTH playing a central role in calcium and phosphate homeostasis. Disorders of the parathyroid gland, such as hyperparathyroidism and hypoparathyroidism, can lead to serious metabolic, skeletal, and renal complications, highlighting the importance of these small but crucial glands in overall health.
(ikram baig)













0 Comments